- Frazis Capital Partners
- Posts
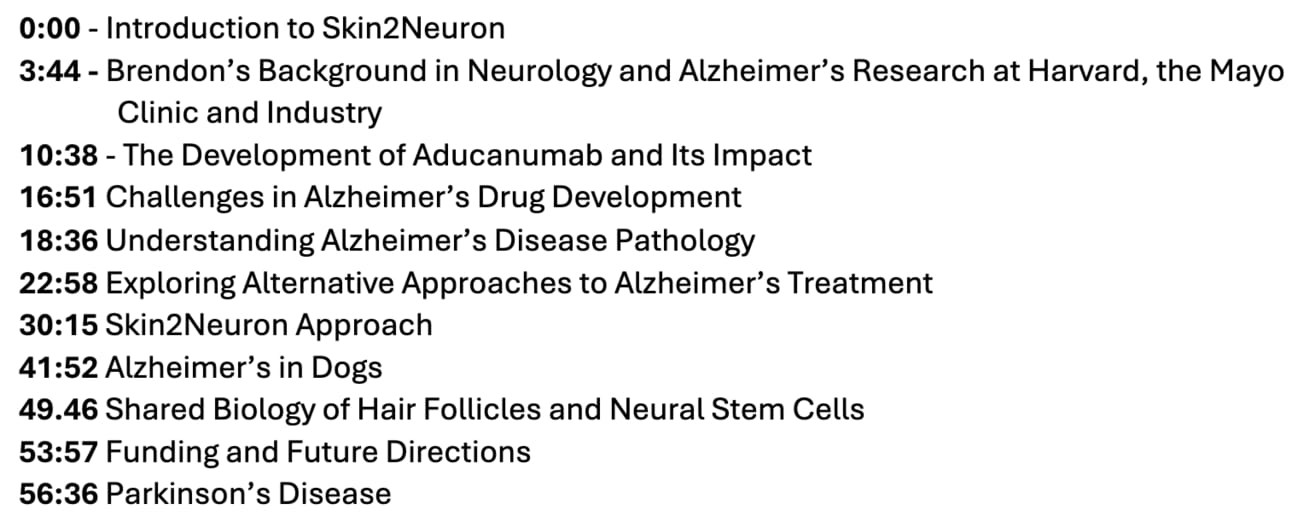
- A cell therapy Curing Alzheimer's in dogs and people
A cell therapy Curing Alzheimer's in dogs and people
"This is the second time in my career when I've looked at something and said, ’this is what I want to work on’."
I had a fascinating conversation with Dr Brendon Boot, CEO of Skin2Neuron, whose cell therapy reversed dementia in dogs.
We invested in their current round through our venture fund alongside a number of specialist biotech investors. If you want to speak to the company let me know and I can put you in touch.
Brendon was a neuroscientist at Harvard and the Mayo Clinic, and was the Medical Director of Biogen’s Phase Ib trial of aducanumab, one of the most closely watched studies in Alzheimer’s and healthcare.
Unlike most approaches to Alzheimer’s which aim to slow decline, Skin2Neuron’s cell therapy actually restored function in dogs with dementia. The dogs ultimately died of unrelated causes, and autopsies showed the injected cells had integrated into the brain and migrated to where they needed to be.
In biotech we focus on companies that do their own science and have potentially curative outcomes, and this company was built on work done here in Sydney by Michael Valenzuela and increasingly international collaborators.
Most animals are poor models for medical research, and this is particularly true in Alzheimer’s, a disease of the organ perhaps most distinct in humans. It appears at an age that very few mammals reach.
Domestic pets are the exception, perhaps because they share an environment with us and live to old age.
As it turns out, 68% of dogs aged 15+ get dementia, and it presents with the same biochemical changes and protein aggregation seen in humans (for a summary see ‘A canine model of human aging and Alzheimer’s’).
In oncology, animal models can be as crude as inducing or engrafting human tumors onto rodents. Many drugs that work in these models don’t work in humans, and it’s likely that many potential drugs have never been pursued as they failed at this stage.
Working with a naturally occurring large mammal model greatly increases the chance that success will translate to humans. And as this is a cell therapy, rather than a small molecule, the likelihood of success is also higher than a typical drug.
Skin2Neuron’s cell therapy takes rare cells from a patient’s hair follicles, converts them to neuronal precursor cells, then implants them in the brain. Here, they self-organise, move to where they need to be, and restore function.
It might seem strange that hair cells can be converted into precursor neurons but it turns out both form from the same original cells in the embryo.
Like hair, new neurons are generated throughout our lives in the brain, and this is the role these cells play.
Many treatments work in animals but never make it to the clinic - why be confident this might work in humans?
Consistently translating drugs that work in cell cultures and animal models into human patients is an unsolved problem. We are a long way off having computer models of people, though perhaps we will seem them in our lifetimes.
Evolutionary distance between species leads to subtle changes in key proteins all around the body that change the shape of molecules just enough to make animal-to-animal comparisons difficult, especially for subtle diseases like cancer which require precise targeting of a patient’s own tissue.
As a cell therapy that works in large mammals, however, there’s better chance of success than a small molecule drug.
Alzheimer’s and other diseases of aging are particularly difficult for drug development given the long timeframes involved. It’s all but impossible to run consecutive trials that might take ten years or more.
Every year adds substantially to the cost of a trial, and patents run out too.
In this case, if the treatment works as it did in dogs, and a patient’s own cells engraft into the brain and increase function, the results should be clear quite soon afterwards.
And if a cell therapy works in a small number of patients, it’s likely to translate into larger trials and the broader patient population. So for a number of reasons, this is the most promising Alzheimer’s opportunity I have come across.
Podcast Transcript
Michael Frazis
Brendon, you've got a distinguished background in the sciences and Alzheimer's. Why don't you tell us about yourself?
Brendon Boot, S2N CEO
Sure, I'm a neurologist by training.
I trained here and in France, at the end of my training, I got some great traction and scholarships at the Mayo Clinic where I did a fellowship focusing on degenerative brain diseases.
From there, I was lucky enough to get an academic position at Harvard.
I spent 11 and half years at Harvard, and about halfway through that I made the transition to industry. I kept my academic role so I could still treat patients and teach fellows, which I've been doing that since 2014.
It was kind of an accident that I got into industry.
I was happy working on research into predictors of prognosis in Alzheimer’s and Parkinson's based on genetics, PET scans, etc.
Michael Frazis
So, in other words, what determines the likelihood of progression after a patient is diagnosed?
Brendon Boot, S2N CEO
I was looking at risk genes to determine whether they correlate with prognosis across different diseases. We analyzed early changes using MRI and PET scans to predict which patients were likely to do well or not.
An important factor when developing a drug is to find candidates who have the same prognostic or disease course.
At that point I got a call from Biogen, who are heavy in neurology.
They had data for the first ever post-treatment scan for the drug Aducanumab, now Aduhelm.
It was perhaps the most effective monoclonal antibody directed against beta-amyloid, a protein that collects in the brains of people with Alzheimer’s.
Aduhelm is a monthly injection that binds to the beta-amyloid and removes it from the brain. Beta-amyloid is known to accumulate in somebody with Alzheimer’s for about 15 years before they get their symptoms.
It would be really exciting to be able to remove it, which is what they showed me.
In the first post-treatment radioligand design PET scan, on the first patient, the bet-amyloid was gone.
Michael Frazis
So, Aducanumab effectively cleared the beta-amyloid?
Brendon Boot, S2N CEO
Yes. I looked at that scan and I said to myself, ‘I've got to keep a poker face here. I don't want these people to know I'll work on this for free’.
It was a revelation at the time.
It was the only promising target in the entire industry for Alzheimer's disease and luckily, I got the job.
I was the medical director for that phase one study and working on the phase two and three programs. It was a baptism of fire, really.
The drug was very effective, but it also had a lot of off-target toxicity that creates an inflammatory reaction.
That inflammatory reaction could have some rare but severe consequences. What was common was an extraordinary change on the MRI, which indicated the inflammatory response. I was involved in working out the predictors of that inflammatory response, working out titration regimes so that we could gradually increase the antibody to decrease the chance that we overcook that inflammatory response.
Michael Frazis
What happens if that inflammatory response gets out of hand?
Brendon Boot, S2N CEO
A couple of folks ended up in the intensive care unit.
You can get a secondary haemorrhage as late in the disease beta-amyloid collects around the blood vessels as well. If you have an inflammatory response, the blood vessel ruptures. It's epileptogenic, quite a few people have had seizures. We also saw headaches, confusion, etc.
Fortunately, nobody passed away in that study, but it put some grey hairs on my head. It was great learning process for me to understand how to guide people through serious clinical trials and to work in large teams to minimise risks.
At the same time, we were developing another drug with the same mechanism and target through Eisai.
Eisai is a large Japanese pharmaceutical company who had a long history in Alzeihmer’s. They're the ones who developed Aricept donepezil which is the most used symptomatic treatment.
Michael Frazis
Which symptoms does that treat, in Alzheimer's?
Brendon Boot, S2N CEO
It basically augments your memory.
It doesn't change the course of the disease. Some data suggest a minimal change, but it does improve your immediate memory. It's modest as well, a 1.4 point improvement on a 30 point scale. The interesting thing is they were a very conservative company.
That was a real distinction to the corporate personality of Biogen, which was quite aggressive. I got to work on both programs and it was really helpful to get those different perspectives.
In the end, both of those treatments came to market. They had a co-development and a co-marketing arrangement.
Michael Frazis
What happened with that?
Brendon Boot, S2N CEO
I know a lot more about it than I can really share.
What can I tell you is that they were very aggressive in what they were trying to do.
Back then, 2014 through 2016, a few of us there, neurologists in particular, said the clinical effect that we saw in those early phase trials was an overestimate.
So, we struggled to convince senior folks to be less aggressive going forward. In the end, the first phase three trial was positive. One of the phase two trials read positive and the other read negative.
The argument they made was that it was the delay in the change in the titrations.
I was involved in a titration regime that gradually eased dosing, which was later implemented and linked to reduced exposure in a negative outcome. The FDA advisory committee recommended against approval, but the FDA ultimately gave approval based on positive PET scans showing reduced exposure to the monoclonal antibody.
The product was marketed and accepted in the neurology field, followed by Eisai’s and Lilly’s which are both still marketed in the US and Europe.
Michael Frazis
How strong is the efficacy in those two other products?
Brendon Boot, S2N CEO
Marginal. And the effect is a bit smaller than what we would say is a minimally clinically important difference. You couldn’t see a difference if a patient was on it for 18 months. But if you looked over the 1700 people that might be in one of these trials, you can see a difference.
The difference increases with time, the medications and the mechanism - it comes down to the development process. We’ve had to wait until somebody has symptoms to use this treatment to demonstrate improvement.
But these are medications that should be directed very early. This should be a secondary prevention model, which is what these companies are doing.
When you develop beta-amyloid, it takes 15 years to show symptoms. Then a second pathology called tau arises which indicates a steady decline.
Comparable to treating someone’s cholesterol after their first heart attack, beta-amyloid should be treated the same way. Earlier in the diseases before symptoms.
There are currently trials with Eli Lilly and Eisai to treat people with beta-amyloid to delay or even prevent symptoms. Data suggests that's going to be the case.
I think in that context, a significant positive effect is greater.
Give it five years, I think anyone who hits 50 will get their faecal occult blood test in the mail and an invitation to have a plasma screening for this protein.
Following that will be subcutaneous formulations and potentials for oral therapies.
I think this will be a new treatment regime for this disease that's going to prevent a lot of misery.
Michael Frazis
It does highlight the challenges with this; it's very slow, symptoms show up relatively late in the disease progression making it difficult to design trials for.
There's always hope it could work earlier in disease progression, but how do you achieve that? What are the challenges around timeline, funding and IP?
Brendon Boot, S2N CEO
It all comes down to capital's time horizons.
If you're a venture capitalist, biotech or pharma, you need to have a time horizon of 15 years. That's rare for small companies and even large ones like Biogen.
Companies like Eisai, Lilly or Roche, can afford that luxury. In 2014 a lot of us were advocating to do a symptomatic trial, but also a secondary prevention trial.
Michael Frazis
There's a lot of controversy around the beta-amyloid hypothesis.
What's the current best understanding of how this disease develops and what causes it?
Brendon Boot, S2N CEO
Some still argue that beta-amyloid research has been a waste, but that’s no longer defensible. Three large phase 3 programs have shown it is possible to change the course of the disease. It can be slowed if symptoms are already present.
All of the genetic risk factors load on beta-amyloid or microglial genes. I think anyone who argues that it's not heavily involved in the pathological process is not being honest with themselves, there are secondary aspects.
Microglial cells are brain immune cells that support neurons or respond to infection. Many Alzheimer’s risk genes are expressed in microglia, suggesting their role in both managing beta-amyloid and reacting to infection.
When you look at other risk genes that aren't directly involved in the precursor or processing of beta-amyloid, a lot of them are expressed by these cells.
Data shows that chronic infection, viral infections in particular, increase your risk of Alzheimer's disease. For example, studies show that herpes zoster (which can cause shingles) increases risk, but vaccination reduces the likelihood of developing Alzheimer’s. Similarly, herpes simplex virus has an elevated risk of Alzheimer's and other forms of dementia, but the oral medications brings that risk back down to the population average.
Michael Frazis
What are the other approaches?
We can move on to cell therapies and gene therapies.
Brendon Boot, S2N CEO
There's a couple of small molecules bouncing around the Alzheimer's field. Most of the work is underwhelming, if you ask me.
There are a few kinase inhibitors around. A lot of these have been tried in the past, there is work on the second protein that accumulates in the brain called Tau.
Tau starts to accumulate inside the cells when symptoms arise. This gets phosphorylated and then accumulates, it's a very sticky protein. It will stick to itself and accumulate inside the cell.
I'm less excited by that because Tau is a protein that forms on something called a microtubule, which is the scaffolding for a neuron. Neurons can be incredibly long and incredibly thin, so they need a very strong scaffolding process.
For example, a neuron can be as long as a piece of wool stretched between New York and Boston. It can be that thin, but that long. You need these kinds of proteins to hold them together.
Michael Frazis
So, the neuron is wrapped around in your brain, connected to other neurons?
Brendon Boot, S2N CEO
Yes, there's a number of potential connections in the brain is as 10 with 17 knots behind it. A huge number of potential connections.
Michael Frazis
It's almost 10^17 parameters as AI people might say.
Brendon Boot, S2N CEO
Exactly. This concept of Tau being pathological, there's an idea that if it breaks up it can make another Tau protein stick to itself.
Given its structural role, it may be a consequence of the cell's destruction due to other processes, perhaps unleashed by beta-amyloid.
There are mixed results in those tail monoclonal so far.
In cell and gene therapy, there's a couple of gene therapy programs out there. Usually they're trying to modify these risk genes. The major risk gene is called APOE, it affects the confirmation of something called amyloid precursor protein, which is the precursor to beta-amyloid.
If you carry the fourth allele, APOE4, you have an increased risk of getting Alzheimer's disease. Whereas if you have APOE2, you have a decreased risk.
A lot of these programs are trying to change people's confirmation through editing or canonical gene therapy increase the relative amount of APOE2 above 4.
Michael Frazis
These are all clues as to how the disease actually works as well.
What are those genes involved in?
Brendon Boot, S2N CEO
The amyloid precursor protein sits across the membrane of a neuron and is involved in signalling responses to inflammation. It’s the major risk gene.
Michael Frazis
How did gene therapy work in this case?
How could you edit all the cells in someone's brain?
Brendon Boot, S2N CEO
After Biogen I worked for Voyager Therapeutics, a gene therapy company out of Third Rock. We focused on Parkinson's disease and a tau program. Our approach was unusual – we developed a vectorized monoclonal antibody.
Since monoclonal antibodies don’t easily reach the brain in high concentrations, we engineered a capsid that, once injected, delivers DNA into neurons.
These neurons then produce the antibody targeting tau. In other cases, similar vectors can be used to express proteins that modify disease-related proteins like APP.
Michael Frazis
APP being Amyloid Precursor Protein.
Brendon Boot, S2N CEO
Exactly. The challenges there are the same as we were talking about. When you're going to do that, you have to wait a long time to see a clinical effect. Those kinds of clinical effects are going to be long, slow development programs.
Given we had a massive effect with the Biogen monoclonal antibody, just stripping the brain of that stuff. What we're talking about with these gene therapies is an early manipulation.
Michael Frazis
Why don't we move on to Skin2Neuron?
How did you get involved in the company and could you give us some background on what you do?
Brendon Boot, S2N CEO
It's been a journey.
I went from working on aducanumab at Biogen. I realized that synuclein was going to be the next important pair of modalities. With that I went to Voyager, did a couple of Phase One studies there in Parkinson's disease. After that, I consulted with a group called SSI, which is like a plug and play biotech team consultancy firm in the US.
I ended up with an independent client, Blue Rock Therapeutics.
Blue Rock was a cell therapy company. And I consulted, loved it, joined them. And not long afterwards, we were acquired by Bayer.
There we did cell therapy in Parkinsons.
This was an embryo-derived pluripotent stem cell that we use to inject in the brains of patients with Parkinson's disease, essentially making a cell that would eventually produce dopamine to replace the lost dopamine.
I spent a couple of years with them ⁓ before making my decision to come back home. I was lucky enough to have developed a good relationship with a venture capital firm down here called the IP Group, with the idea that we went all around Australia and New Zealand looking for interesting technology.
By far the most exciting thing I found was Skin2Neuron.
Ironically, it was about two blocks away from where I was sitting. Having spent all that time over in Boston, the most exciting cell therapy opportunity on the planet was right there.
It was unique in quite a few ways.
Firstly, it's not a pluripotent cell. It's a what we call a unipotent neuronal precursor.
A lot of the challenges with cell therapy is that you're taking a cell and pushing it back to believe that it's the first ever cell that you have worked. It's an induced pluripotent stem cell. You do that with the things called the Yamanaka factors - there are four factors, four genes.
Oncogenes are cancer-causing genes. When you introduce them into cells and begin replicating those cells by plating them and allowing them to grow, then expanding them across more plates, you increase the risk of selecting for cancerous mutations.
This is a major concern with induced pluripotent stem cells (IPSCs), they are powerful disease models but carry serious risks as therapies due to their potential for uncontrolled growth.
At Skin2Neuron or S2N as we prefer to call it now, is a cell that is not from that lineage.
It's already dedicated to becoming a neuron and it can't make copies of itself ad infinitum. It's much safer. The other exciting factors is the data. I can show you some slides on the histology.
What's unique about S2N is the approach.
Most people think that you're born with all the neurons that you'll ever get or that you don't make any new ones when you're an adult. That's not true in two parts of your brain. One involved in your sense of smell and the hippocampus, which is what we’re interesting in. The hippocampus is the memory center of your brain where you make about 700 new neurons a day.
If you've Alzheimer's disease and when you get old, you lose more cells than you make. Creating a 10 million cell deficit in the part of the hippocampus called the CA1.
What's exciting about S2N is that we've found this unipotent neuronal precursor.
It's a very rare cell in your hair follicles. We isolate and expand those then use a neurosurgical injection to inject them back into the hippocampus.
Michael Frazis
Is that unusual? Is that a surprise that it comes from you’re a hair follicle?
Brendon Boot, S2N CEO
It is. Our scientific founder, Michael Valenzuela, developed an interest in canine Alzheimer's disease: dogs get Alzheimer's disease. At the same time a lot of folks had been focusing on skin and the pluripotent stem cells there.
When Valenzuela was taking skin, he worked out that the cells that he was getting were coming from the hair follicles and not from the other parts of the skin and the dog.
Michael Frazis
Interesting.
Brendon Boot, S2N CEO
When you inject them in the hippocampus, they replace the connections between neurons and reconstitute the memory circuits.
The bottom left of the figure, is the second time in my career when I've looked at something and said, ’this is what I want to work on’.
I had the same feeling about that image as when I saw that PET scan back at Biogen.
I've been in cell therapy long enough to see that if you have a beautiful looking graft, you can have an extraordinary clinical effect. These graphs are extraordinary. You're looking at human stains in rodents. On the top, it's a model of Alzheimer's disease and a mouse in the bottom.
You can see the injection tract here in this figure.
When I look at the work that we were doing at Blue Rock, you're used to seeing just the injection tract and then a few cells collecting around where they were injected.
They might spread out a little bit, tiny amounts over months, but these cells follow chemotactic gradients and reinsert themselves into the anatomy.
There's that CA1 field, the pink is the cell bodies, and the yellow/grey is a marker of synapses connections. These cells have followed these gradients to organize themselves into to recapitulate the structure.
Michael Frazis
So, you might have expected to see just red around that injection channel, but now you're seeing them spread out and integrate?
Brendon Boot, S2N CEO
Yes. Even down to the microstructure, they look exactly the same.
More importantly, what we've been able to show is that you can stimulate the host tissue and make the graft neuron fire. It’s functionally integrated as well and reconstituted the circuit. An extraordinary finding.
We’ve done lots of work on rodents, but rodent models of Alzheimer's disease are terrible. They don't predict what happens in the clinic. This is why there's been so many failures of candidates because rodent work doesn’t translate to humans as rats don't spontaneously develop the pathology or symptoms of Alzheimer's disease.
Michael Frazis
I guess our brains are what makes humans distinct, so it’s going to be hard to replicate.
Brendon Boot, S2N CEO
The other thing that made me fall in love with this company is that the founder (Valenzuela) spent eight years doing preclinical work in the only valid large animal model of Alzheimer's disease. The dog. Dogs get Alzheimer's disease.
Michael Frazis
Why do think dogs are such a good model compared to other large mammals? Could it be due to their close proximity to humans and shared environment?
Brendon Boot, S2N CEO
Good question, I don't know if I have a good answer for you.
I do know that dogs have the same risk genes as humans. APOE4, the major risk gene for Alzheimer's disease is conserved between dogs and humans.
Only a small fraction of humans have APOE4 in two copies of it, but all dogs do.
Combined with the fact that they can live to longer ages now probably increases risk. What Valenzuela did was exactly what we're going to do with humans in 2027.
He took elderly dogs that had memory syndrome.
That's photos of the patients and their ages – all people's pets in Sydney.
Michael Frazis
How do you know if Alzheimer’s is present in dogs?
Brendon Boot, S2N CEO
They have a combination of different kinds of behaviours.
They can get confused, stop recognizing their food, get lost in the house, get lost outside of the house, they'll stare at walls. Just like humans do, they have something called sundowning, where they become confused around sunset.
They'll have nocturnal wandering, lose their sense of smell, start to soil the house where they didn't before. It's a big consolation of symptoms. Some of them become quite episodically aggressive.
This trial took him eight years, and it is basically the same thing as we'll do in humans. Take hair follicles and use our process to isolate, enrich and expand them.
You can see in the MRI the little red dots which are the target areas in the hippocampus where we put these cells.
This is a neurosurgeon who operates on humans out of Westmead Hospital, performing the surgery with a standard stereotactic frame and our founder assisting her.
The results are extraordinary.
Data showing that there was a non-standard deviation increase in the density of synapses, so connections between the neurons. That was only found in the areas where the dogs were injected. It was found even though the dogs had beta-amyloid and tau pathology, proving that they did that Alzheimer's disease.
Some objective improvements. This is a sand maze, there was a reward object hidden in the sand. The dogs were better able to go straight to that and remember where it was, even after a delay. Less of nocturnal wandering and that kind of thing.
Rating scale, like the one we use in humans, called the canine CDR. How many of those symptoms and the frequency - these results are extraordinary.
They're huge, they're meaningful.
Three out of the five dogs that got the treatment went back to normal within the normal range at about the three-month mark and then stayed that way for up to two years.
All of the dogs were euthanized up to two years later, but for reasons other than a return of their dementia syndrome.
That augurs really well for this to be a durable treatment in humans.
Michael Frazis
That is surprising. Nothing is curing Alzheimer's, right? Or even returning function as far as I'm aware, even the best trials have only shown a slow in decline.
Brendon Boot, S2N CEO
Yes, we can't treat a dead cell, and we're not, we're putting new cells in there.